Meld je aan voor onze nieuwsbrief
Bij het aanmelden ga je akkoord met onze Privacy Policy
Introduction
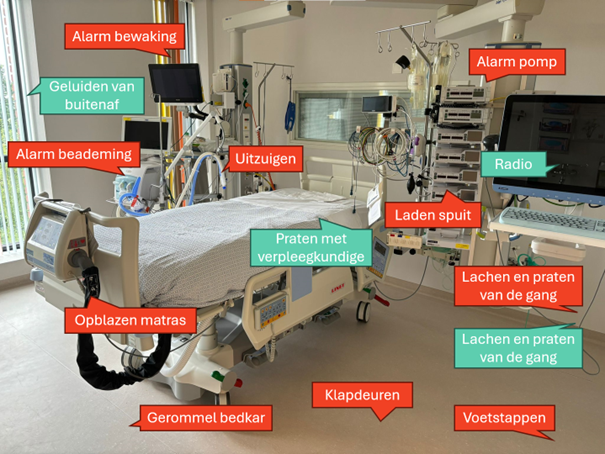
Prolongation of the corrected QT interval (QTc) can lead to Torsade de pointes. Risk factors for the acquired form of prolonged QTc include older age, female sex, low body mass index, electrolyte disturbances, heart disease (ischemia and heart failure) and use of QTc prolonging drugs. Since 2008, new software is available to measure the QTc interval continuously. Research proved these measurements to be accurate and stable. The aim of this study was to determine the frequency of QTc interval prolongation in critically ill patients.
Methods
In a prospective cohort study continuous five-minute QTc measurements of fifty consecutive patients were collected. Inclusion criteria were: (1) age ? 18 years, (2) expected length of stay ICU ? 24 hours. We excluded patients with a widened QRS complex, ventricular pacemaker and bigemini rhythm. Included patients received continuous QTc measurements by the Philips Healthcare software. The Bazett formule (QTc = QT /? (RR)) was used to correct the QT for heart rate. QTc prolongation was defined as more then >500 milliseconds, lasting for at least 15 consecutive minutes. The QT variability index (QTVI) was used to evaluate QT/QTc variation.1
Results
We analyzed 50 patients with in total 3690 hours of continuous QTc interval measurement. 52% of the patients had a prolonged QTc interval. In a single patient 0.2 to 91.3% of the QTc intervals over time was prolonged. The APACHE and SOFA scores were significantly higher in patients with a prolonged QTc interval. The QTVI was significantly higher in patients with a prolonged QTc . We observed one Torsade de pointes in the prolonged QTc group.
Conclusion
The present study showed that QTc prolongation is common in critically ill patients when monitored by continuous QTc measurements. Duration of QTc prolongation is highly variable. Severity of illness and QTVI is higher in these patients. Continuous QTc monitoring can be used to recognize all episodes of prolongation. It needs further study to determine whether a prolonged QTc of fifteen consecutive minutes is relevant or that a longer period is more associated with clinical outcome. In addition, it is still unclear what actions nurses and physicians should undertake other than be aware and reduce QT prolonging drugs.
1 Berger RD, Kasper EK, Baughman KL, et al: Beat-to-beat QT interval variability: novel evidence for repolarization lability in ischemic and nonischemic dilated cardiomyopathy. Circulation 1997; 96:1557-1565